
TL;DR
Heart failure doesn't wait for quarterly appointments, but specialty care still operates as if it does. The result: 200,000+ preventable HF readmissions annually, persistent GDMT gaps, and burned-out cardiology teams managing disease they can't see between visits. This blog shows how AI-powered continuous care infrastructure is rewriting the rules: making the space between appointments clinically visible, operationally manageable, and financially sustainable.
In rural North Dakota, a 58-year-old man named Chuck collapsed while playing basketball. What saved his life was not a single intervention, but a chain of events that held together under pressure.
A bystander trained in AED, teammates who started chest compressions, and a rural emergency department stabilized him. Later, an air ambulance carried him 60 miles to a tertiary cardiac center.
Chuck survived because geography, staffing, and timing all happened to align that night. Had he collapsed at home on his farm, forty minutes from care, the outcome would likely have been very different.
But, this is not the story that repeats thousands of times daily across American healthcare. The real story, the one that takes months to unfold instead of minutes, happens in the space between visits for millions of people living with heart failure, advanced coronary disease, and chronic cardiometabolic conditions.
That story is quieter, harder to see, and it is where specialty care is failing right now.
Specialty cardiology was built for encounters. That design failure now drives preventable admissions, slow medication titration, and invisible deterioration between visits.
Over the last decade, health systems layered remote monitoring, care management, and dashboards onto that model. But accountability still resets every time the appointment ends.
The problem is the architecture. Until the operating model owns continuity, not just visits, performance plateaus no matter how many tools are added.
Story Health by Innovaccer was built to solve that problem. Not as a tool to sit alongside existing workflows, but as the infrastructure that holds risk when there is no visit on the calendar. It does four things that map directly to the continuity challenge.
Home blood pressure monitors, connected scales, symptom surveys, medication histories, and lab results stream into an EHR-native view. Clinicians do not log into a separate system, reconcile spreadsheets, or chase PDFs. Live data appears in the same record they already trust, with real-time updates and a single longitudinal timeline.
Story Health maintains continuous clinical responsibility between visits by evaluating patient vitals, labs, symptoms, and medication data against individualized clinical goals aligned to guideline-directed medical therapy.
The platform translates longitudinal signals into a prioritized view of patients who are not meeting defined clinical goals, enabling remote medication titration and therapy optimization without waiting for the next appointment.
When action is warranted, the AI recommends next steps based on full clinical context and current ACC/AHA guidelines, with transparent reasoning behind every recommendation. Clinicians review, modify, or override each action, while the platform manages ongoing gap identification and follow-through in the background.
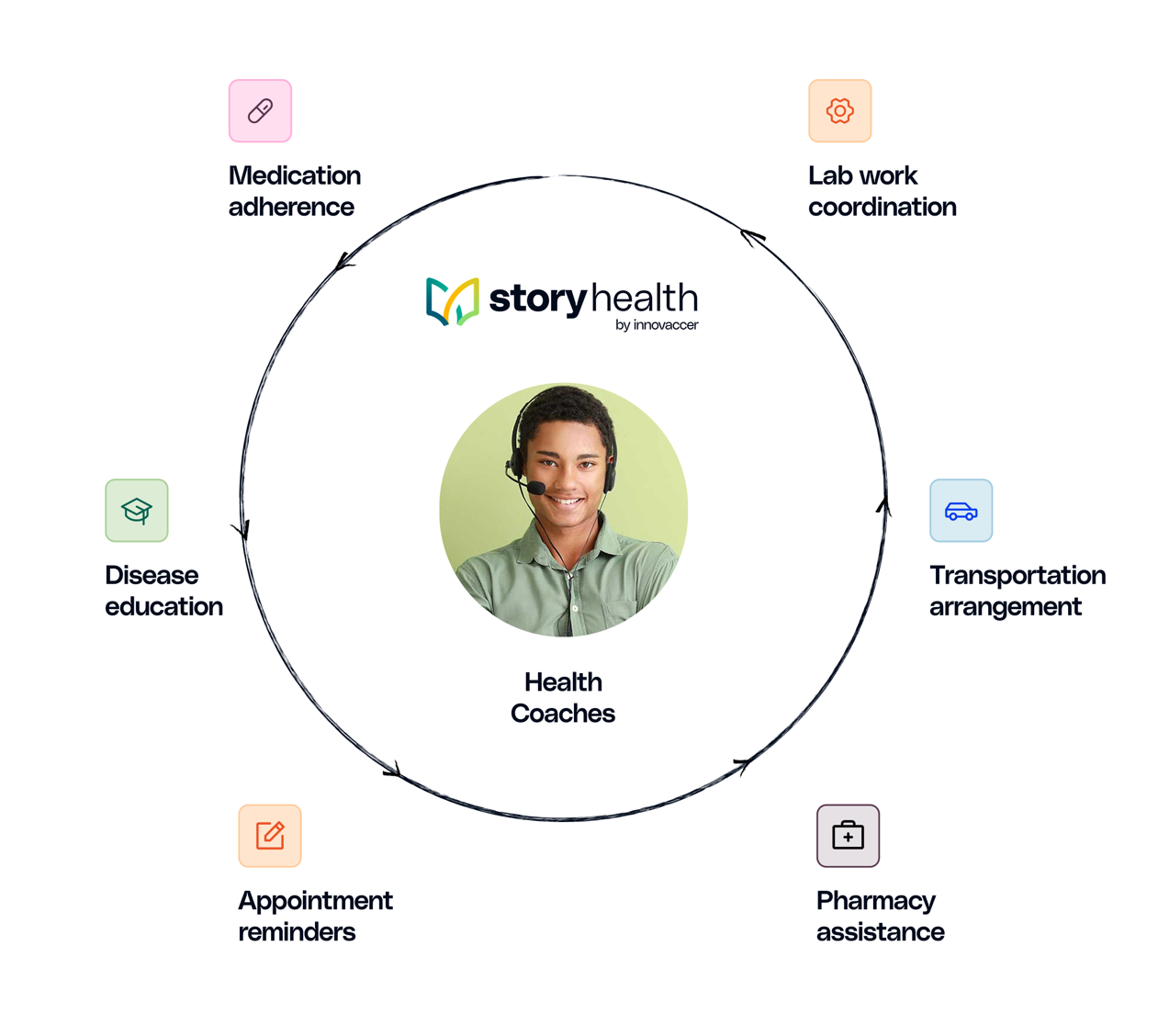
Health coaches operate inside the same system and are deployed proactively. When clinical signals drift, engagement drops, or tasks go incomplete, the platform routes outreach automatically.
Coaches support with medication adherence, guide lifestyle changes, coordinate labs and transportation, and resolve pharmacy friction through structured protocols. This happens quietly through the patient engagement channel , integrated into the patient’s routine. It is an execution layer that absorbs routine work before it escalates into clinical load.
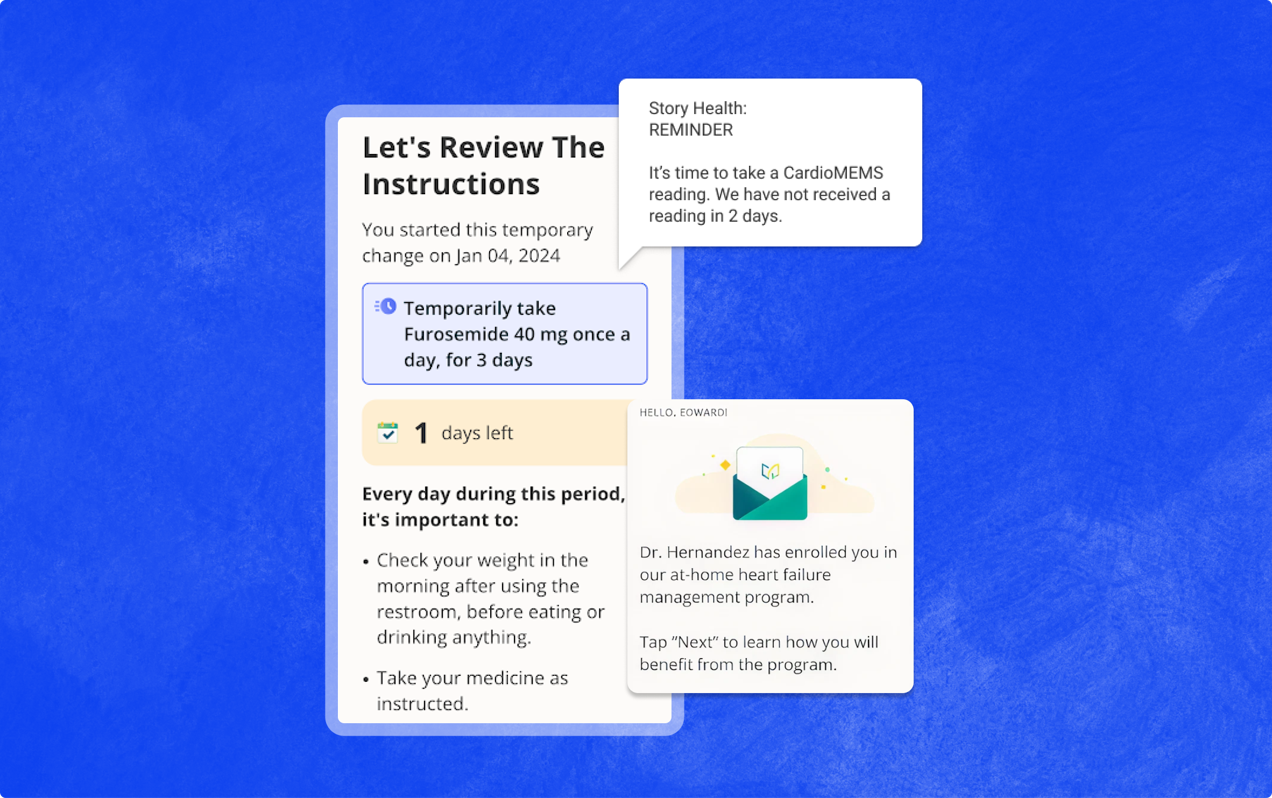
The Story Health patient app delivers individualized daily tasks, reminders, and education. Patients record weight, symptoms, and readings in a guided way. They receive clear instructions when medication doses change, know when labs are due, and can reach a health coach when they are unsure.
In active programs, daily engagement rates sit around 85 percent, no-show rates under 5 percent, and patient satisfaction measures increase materially compared to usual care.
Story Health's AI operates under explicit governance principles. Every recommendation displays its clinical reasoning and data sources. Care protocols align with ACC/AHA guidelines and update automatically as evidence evolves.
More importantly, clinicians retain full authority to override any AI-generated suggestion. The AI advises, but humans decide.
This approach aligns with ONC HTI-1 requirements and FDA guidance on AI transparency, so decision support is transparent, inspectable, and governable in production environments.
Alt text: AI-powered care model implements GDMT optimization to improve Intermountain Health’s health failure patient outcomes
Across seven US health systems, including leading academic centers, patients with heart failure were randomized to either usual care or a remote digital intervention powered by Story Health by Innovaccer.
Patients achieved significantly faster titration than usual care, with Heart Failure Collaboratory scores improving by 2.2 vs 1.4 (p=0.007). 80% of medication changes occurred without visits, and no safety trade-off was observed.
The implication is operational: care does not improve by adding clinics, it improves when responsibility extends beyond the visit.
Read more about the VITAL-HF trial here.
Chuck survived his cardiac arrest because every element of acute intervention aligned in the right sequence at the right moment. Cardiology specialty care demands the same precision, but across thousands of moments that unfold quietly between appointments. Not by chance, but by design.
Story Health's infrastructure makes that alignment possible. The few systems that have incorporated Story Health by Innovaccer, have moved from reactive crisis management to proactive, sustainable care.
The question is how quickly this becomes the standard rather than the exception.
To see how our holistic and intuitive operating model works inside your EHR, request a demo.